How to address gut sensitivity with your child
In an earlier blog, we covered off on the early life and sensory factors that could increase the likelihood of some children having sensory issues with foods that are related to gut sensitivity.
In this post, we focus on some of the ways to address gut sensitivity with your child. Here is our stepwise process towards your child having a less sensitive gut, less ‘melt downs’ related to food and eating, less meal-time stress for parents and more food enjoyment in your household.
1. Avoid food allergy testing that is not evidence-based.
Talk to a dietitian about what can and what cannot be diagnosed from food testing, or have a look at this excellent resource from ASCIA.
2. Gauge whether your child has sensory food issues that could be addressed before, or alongside the gut sensitivity.
Does your child:
- Have a very limited food range (say 20 foods or less)
- ‘Melt down’ if they are asked to try (or even see or smell) a food that is not in their food range
- Take a while to reintroduce a food that they refuse but previously liked (food jag)
- Have preferred foods that tend to be in one colour or texture range?
If you answer ‘yes’ to most of these, it would be best to get some personalised advice from an “SOS’’ trained dietitian. You may also consider a referral to the Child and Family Team at your local community health centre.
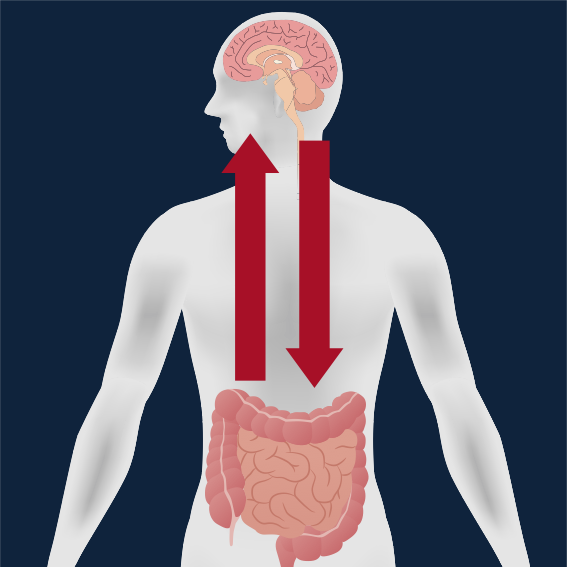
3. Next, we decide if a ‘gut-brain’ or ‘brain-gut’ approach might suit better.
If your child’s gut issues seem to relate to specific foods then a ‘gut-brain’ approach would be our ‘best bet’ whereas if their gut symptoms seem to relate to stress and anxiety we would recommend starting with a ‘brain-gut’ approach.
4. Snapshot of gut-brain strategies.
If you are confident that certain foods affect your child’s gut symptoms, then it makes sense to make some dietary changes. But what do you try first, and how do you tell what has worked?
Our dietitians would first discuss your child’s symptoms as this tells us whether their gut is drawing too much fluid, creating too much gas, or moving food through to quickly or slowly. This would give us clues to which foods to adjust first.
We may trial a ‘top down’ approach where we remove just a few foods, and see if this helps, or we may recommend cutting back quite a few foods to reduce symptoms, then reintroducing foods one at a time.
We may focus on ‘FODMAPs’ or fibre or food additives. Either way, we would need to tailor this to your child’s food preference and needs.
5. Brain gut approaches.
If your child’s symptoms seem to relate more to stress and anxiety, dietary changes may help alleviate symptoms, but would be a secondary strategy. We would recommend addressing the sensory, nervous system, ‘brain’ side of things first and foremost. Here is an excellent place to start in better understanding how the gut and brain talk to each other.
Finally, to address the million dollar question, is it worthwhile for a child with gut issues to trial probiotics?
There is evidence for and against trialling probiotics, but the ‘against’ are not related to potential harm, just about whether they actually help at all and therefore whether they are worth the money.
On the positive side, there is now fairly solid evidence that Lactobacillus and Bifidobacteria (BB) strains are helpful probiotic, with emerging evidence for Akkermansia and Faecalibacterium bacteria groups. The probiotic most likely to be helpful for children with gut issues would be BB-12 to increase regularity of bowels if a daily dose of 1 billion CFU per day is achieved.
If this all sounds great in theory, but you need a hand in supporting your child to make dietary changes that you think could improve their quality of life, please seek out a dietitian to help implement a suitable, personalised dietary approach.
We offer video appointments across Australia or find an APD who specialises in sensory issues near you.